Great communication between a health professional and their patient is a key ingredient for everyone’s healing process, no matter their age. But for older patients, effective communication becomes even more important, leading to better health outcomes, increased adherence to treatment, and improved diagnostic accuracy.
Older patients make up a large proportion of the people treated in health clinics, and this is only expected to increase over the next few years due to our rapidly ageing population. The World Health Organisation has calculated that the current number of people aged 60 years and older now outnumbers children younger than 5 years, and that by 2030, 1 in 6 people in the world will be aged 60 years or over.
As their physical and mental capacity decreases, older people are much more likely to develop a range of medical conditions such as hearing loss, cataracts and vision concerns, back and neck pain, osteoarthritis, chronic obstructive pulmonary disease, diabetes, depression and dementia, as well as frailty and osteoporosis, urinary incontinence, falls, delirium and ulcers that need regular dressing. Many older adults are also isolated, lonely or anxious, and may struggle with mobility and memory difficulties. This highlights why clear, patient and empathetic communication that builds a strong relationship between older patients and their health providers is becoming more important than ever before.
Simply put, helping to make an older person feel comfortable, respected, listened to, understood, and cared for, and making treatment easy to understand and remember, can help lead to better health outcomes. It increases adherence to treatment, helps to accurately diagnose underlying conditions through trust and honesty, and helps to optimise limited interaction time.
Top Tips For Interacting With Elderly Patients
To ensure your elderly patients feel comfortable and relaxed, and to help to improve the health outcomes of your time with them:
Establish respect
Many elderly patients may prefer a more formal term of address, such as Mr., Mrs., Ms., or Miss, or they may like you to call them by their first name. Ask your patient how they would like to be addressed, and avoid using terms like “Dear”, which may come across as patronising.
Make elderly patients feel welcome and at ease in your waiting room
Take time to make sure you have comfortable seats in your waiting room, with raised legs to help older patients to get out of their seats more easily. Consider installing automatic doors so that older patients with walking sticks, frames or weakness can enter without hassle, and make sure reception staff offer to help out with filling out forms – these could be printed in extra-large font to help those with vision difficulties. Older patients may need extra assistance to be escorted to and from exam rooms, offices, restrooms, and the waiting area, and if possible, encourage your reception staff to check on them often if they have a long wait.
Take a few moments to chat to establish a positive rapport
Once in the exam room, elderly patients will often appreciate hearing you introduce yourself clearly, or reminding them of your role if they’ve forgotten, and chatting to you about their day or themselves. You may want to talk to them about the weather, ask them if they have family nearby, or if they’re originally from this area. This will enable you to ask friendly questions about their families or activities in future interactions to build familiarity and reduce stress. Introduce yourself clearly and do not speak too quickly. Remember – older people are frequently isolated and you may be the only person your patient interacts with on any given day, so your time with them is important. Showing you are interested in them can be therapeutic, build trust, and improve their overall mood and wellbeing.
Ask questions about your patient’s living conditions and daily routines
Ask open-ended questions and look out for clues about your patient’s relationships with family members, living arrangements, financial situation, and attitudes toward ageing and illness.This information could help you to better understand what is contributing to a patient’s concerns and make recommendations that are realistic and appropriate for them. Try to ask questions about their home life during the interview, including aspects like:
- What type of heater do you use in the winter?
- Do you have steep stairs in your home?
- Do you own a pet?
- Can you get to the grocery store or pharmacy on your own?
- Are you friendly with anyone in your neighbourhood?
Also, be sure to ask if anything has changed since the last visit. For instance, if they still have the same living arrangements or have experienced some type of loss.
Be patient and create a slow, peaceful environment
Even though you may be running behind schedule, or aware of other patients in the waiting room, older people may have trouble following a quick barrage or questions or become easily overwhelmed by a lot of information at once. Speak slowly and clearly to give older patients time to process what is being asked or said. They may also speak slowly, but be patient and allow them to express their concerns – this may reveal important information and lead to a more accurate diagnosis. Stay aware of your own speed of speaking and body language, as giving the impression that you’re feeling rushed may lead them to believe they are not being heard or understood, or they may withhold information if they are worried that they are taking up too much of your time.
If your time is limited, you could suggest that your patients prepare a list of their health concerns in advance of their appointments. That way they are prepared and you have a sense of everything they’d like to cover during your time together.
Avoid interrupting
Research has found that on average, doctors interrupt their patients only 18 seconds after they’ve started giving the reasons for their visit, and most patients do not complete their explanation after being interrupted. For older people, they may also lose their train of thought and leave out important information. So, make sure you show from the beginning that you want to hear your patients’ concerns, so that you can gain the full picture of what is happening and form an accurate diagnosis and effective treatment.
Use positive body language and active listening skills
When your patient is speaking, avoid the temptation to face your computer and type up notes. Instead, face your patient, maintain eye contact, and use brief responses to show that you’re listening, such as “Right, okay,” “I see”
Use empathy to show that you care
While listening to your patient, look for opportunities to respond to their emotions and phrases like“That sounds difficult,” or “I’m sorry you’re facing this problem – I think we can work on it together.” This won’t add much time, but it can help older patients to feel cared for and understood, and establish trust – which is crucial for helping them to adhere to treatment.
Avoid unnecessary repetition from the patient
For older patients who are unwell, it can be very tiring if they have to tell their story in detail to one staff member, and then again to another, so try to avoid this as much as possible.
Use everyday language
Even though older people often have multiple ongoing health concerns, this doesn’t mean that they have a lot of knowledge about their disease or understand complex medical jargon. To start, it can help to ask patients what they know about their condition and build on that. Although some terminology may seem common and self-explanatory, such as MRI or CT scans, older patients may be unfamiliar with what these tests mean, so check often to make sure your patient understands what you’re saying and what is happening. It can be helpful to ask them to retell the diagnosis or care plan in their own words, which will help them to remember it as well.
Write down important information
Older patients can become overwhelmed with information and find it difficult to remember diagnoses and how to carry out their treatment, so they can benefit hugely from having written notes to refer back to later at home. Make sure this information is simple, clear, and direct. For example, instead of saying “Avoid being sedentary”, you could say “Stand up at least once every half hour”.
Before leaving, ensure they understand
At the end of their appointment, ask your patient to tell you in their own words what you’ve talked about today, and what they understand about their treatment. This gives you an opportunity to ensure they have understood you correctly, and improve their treatment outcomes.
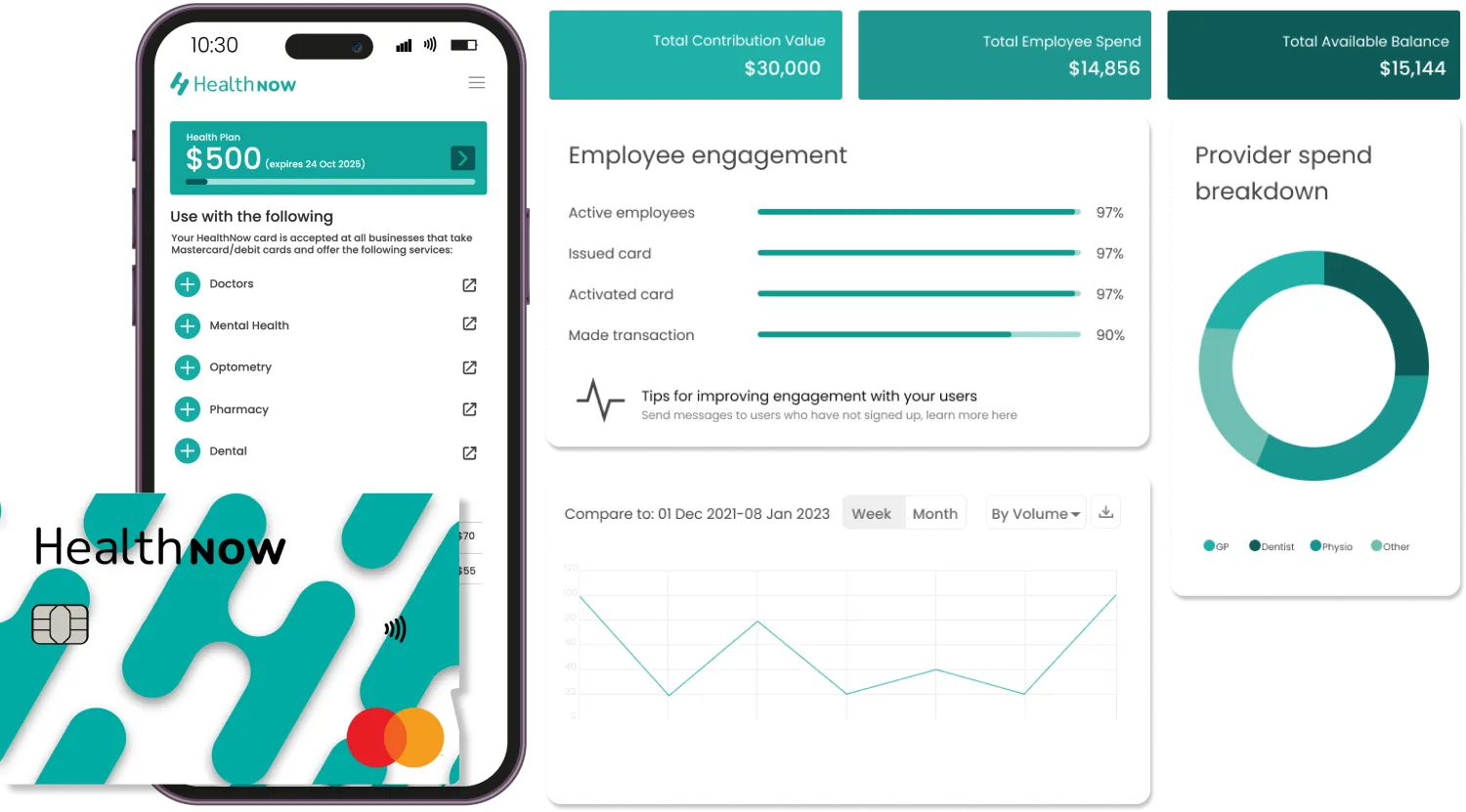
Make The Payment Process Easier And Less Stressful For Older Patients Through HealthNow
Another factor that can overwhelm patients at a medical or health clinic, and distract them from focusing on the key information regarding treatment plans, includes the financial pressure to pay for their initial appointment upfront, as well as any necessary follow-ups or prescriptions. HealthNow is an innovative way of addressing these concerns to leave your patients feeling more relaxed and at ease in your clinic, while also improving accessibility through offering an ethical, health-specific Buy Now Pay Later (BNPL) solution.
HealthNow eliminates the need to offer and manage payment plans by offering a digital solution that is entirely free for your patients, who can choose to split the cost of their health services or products with you over up to six weeks. As you get paid in full on the day of the services by HealthNow, there is no added financial stress putting pressure on your patients, giving them peace of mind to focus on what’s most important during their time with you – their health. HealthNow can also be used anywhere with internet availability, eliminating financial paperwork from accepting payments in remote locations without a dedicated clinic. Additionally, as HealthNow users search their database for the wide selection of clinics that this payment method can be used at across New Zealand, it works as an in-built marketing tool, directing local customers to you without a cent spent on advertising.
When the stress of having to find the full upfront cost is removed, users increase the amount they spend on health products and services which not only helps improve the bottom line for the clinic, but also helps contribute to better long term health outcomes for the patient and improves patient satisfaction throughout the course of their care.
To get started with HealthNow, register your clinic’s interest via this contact form and a HealthNow team member will get back to you promptly.
References:
- https://pubmed.ncbi.nlm.nih.gov/6486600